OmniMD introduces a national BI & Analytics platform giving clinics real-time clinical, financial, and operational clarity to act early and reduce revenue risk.
OmniMD announced the launch of its national-scale BI & Analytics Services, a unified intelligence platform designed to bring clinical, financial, and operational clarity to ambulatory practices across the United States. As clinics face escalating reimbursement pressure, documentation complexity, and operational volatility, OmniMD’s new platform provides the visibility required to make timely, precise decisions.
➤ 𝐀𝐦𝐞𝐫𝐢𝐜𝐚’𝐬 𝐂𝐥𝐢𝐧𝐢𝐜𝐬 𝐇𝐚𝐯𝐞 𝐭𝐡𝐞 𝐃𝐚𝐭𝐚. 𝐓𝐡𝐞𝐲 𝐃𝐨𝐧’𝐭 𝐇𝐚𝐯𝐞 𝐭𝐡𝐞 𝐈𝐧𝐬𝐢𝐠𝐡𝐭
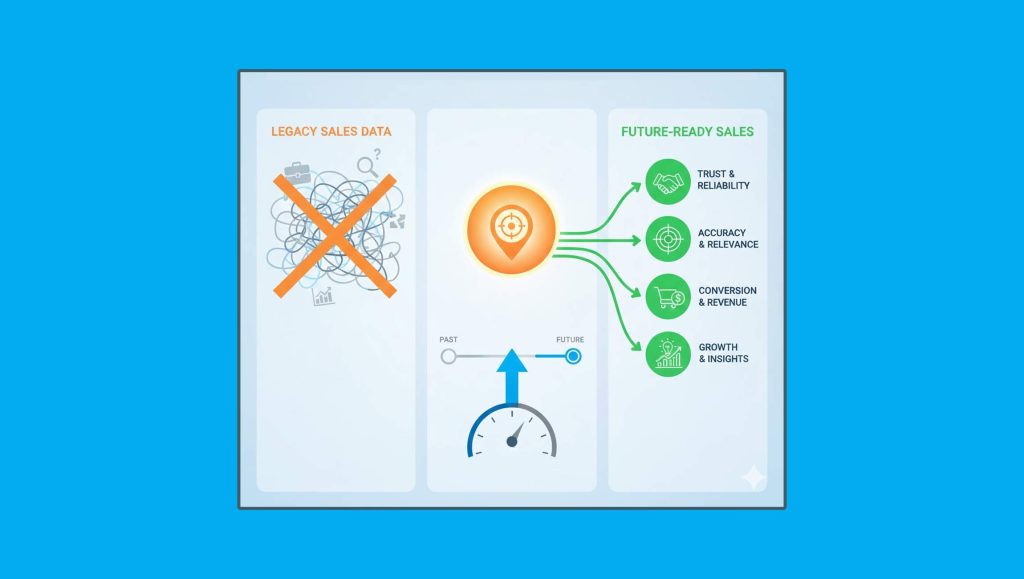
The U.S. healthcare sector generates more data than any other clinical ecosystem in the world. Yet most outpatient practices operate without real-time visibility into revenue risk, care variation, or operational performance. Monthly reports reveal problems after they become costly, and fragmented systems prevent leaders from seeing how issues develop.
National market trends reinforce this challenge. The U.S. healthcare analytics market is projected to reach USD 58.4 billion by 2033 (IMARC Group). Investment continues to rise, but practical intelligence at the clinic level remains limited.
OmniMD’s internal analysis shows that nearly 40% of early revenue-risk indicators do not appear in traditional reporting workflows. Denial-pattern shifts, documentation slowdowns, scheduling bottlenecks, and patient adherence drops often form weeks before leaders recognize them.
Clinical and financial risks form long before they become visible. Our goal is to give clinics the clarity required to act early, adjust accurately, and protect both care quality and revenue stability”
— Divan Dave, OmniMD’s CEO
➤ 𝐀 𝐏𝐮𝐫𝐩𝐨𝐬𝐞-𝐁𝐮𝐢𝐥𝐭 𝐈𝐧𝐭𝐞𝐥𝐥𝐢𝐠𝐞𝐧𝐜𝐞 𝐏𝐥𝐚𝐭𝐟𝐨𝐫𝐦 𝐟𝐨𝐫 𝐀𝐦𝐛𝐮𝐥𝐚𝐭𝐨𝐫𝐲 𝐂𝐚𝐫𝐞
OmniMD’s BI & Analytics platform establishes a single intelligence layer across an entire clinic ecosystem. It provides clear, real-time visibility into clinical, financial, and operational patterns that previously remained buried within disconnected systems.
■ 𝐀 𝐔𝐧𝐢𝐟𝐢𝐞𝐝 𝐂𝐥𝐢𝐧𝐢𝐜𝐚𝐥–𝐅𝐢𝐧𝐚𝐧𝐜𝐢𝐚𝐥 𝐃𝐚𝐭𝐚 𝐅𝐚𝐛𝐫𝐢𝐜
The platform integrates EHR, RCM, billing, scheduling, claims, and patient-engagement data into a normalized data structure. Leaders no longer depend on manual exports or fragmented systems to understand performance.
■ 𝐑𝐞𝐚𝐥-𝐓𝐢𝐦𝐞 𝐑𝐢𝐬𝐤 𝐚𝐧𝐝 𝐎𝐩𝐩𝐨𝐫𝐭𝐮𝐧𝐢𝐭𝐲 𝐃𝐞𝐭𝐞𝐜𝐭𝐢𝐨𝐧
The analytics engine identifies anomalies in payer behavior, throughput, follow-up patterns, and documentation quality. Issues appear at the moment they begin, allowing leaders to intervene before they escalate.
■ 𝐂𝐫𝐨𝐬𝐬-𝐒𝐢𝐭𝐞 𝐁𝐞𝐧𝐜𝐡𝐦𝐚𝐫𝐤𝐢𝐧𝐠 𝐚𝐧𝐝 𝐒𝐭𝐚𝐧𝐝𝐚𝐫𝐝𝐬
Multi-location groups can apply consistent KPIs, governance models, and productivity metrics across all sites. Variability becomes measurable, and expansion decisions become data-driven.
■ 𝐂𝐥𝐢𝐧𝐢𝐜𝐚𝐥–𝐎𝐩𝐞𝐫𝐚𝐭𝐢𝐨𝐧𝐚𝐥 𝐀𝐥𝐢𝐠𝐧𝐦𝐞𝐧𝐭
The system links clinical behavior with operational and financial outcomes. Leaders can see how documentation patterns influence denials, how visit volume affects staffing requirements, and how care gaps impact revenue integrity.
➤ 𝐄𝐚𝐫𝐥𝐲 𝐅𝐢𝐧𝐝𝐢𝐧𝐠𝐬 𝐅𝐫𝐨𝐦 𝐎𝐦𝐧𝐢𝐌𝐃’𝐬 𝐀𝐧𝐚𝐥𝐲𝐭𝐢𝐜𝐬 𝐃𝐞𝐩𝐥𝐨𝐲𝐦𝐞𝐧𝐭𝐬
Initial deployments in medium and large practice groups revealed patterns previously undetected in traditional reporting:
● 22% of denial volume in one network was linked to a small set of payer–code combinations.
● Daily monitoring reduced days in A/R by 9 to 15% within 90 days.
● Documentation friction accounted for up to 12% of provider productivity variation in several sites.
● Predictive adherence models identified follow-up gaps 10 to 14 days earlier than standard workflows.
These insights allowed clinics to intervene earlier, adjust workflows, and recover revenue that would otherwise have been lost.
Read More: The Future Of Sales Training – Which Salestech Platforms Help