End-to-end solution will drive clinical and financial success of value-based care programs
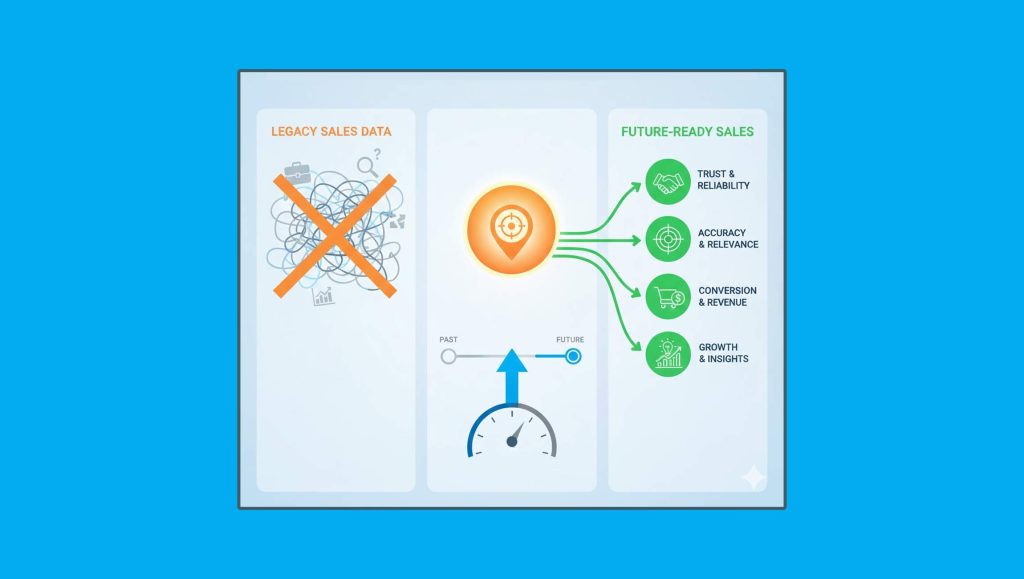
Clarify Health, a leading cloud analytics company delivering real-world insights to healthcare and life sciences organizations, announced the acquisition of the Value Optimization business of Apervita, the trusted platform for healthcare collaboration for payers, providers and other stakeholders. This acquisition bolsters Clarify’s integrated analytics platform for end-to-end value-based contract design, payments reconciliation, clinical performance assessment, and reporting. Powered by the big-data capabilities of the financial services industry and the analytics methodologies of Wins Above Replacement (WAR) in baseball, the Unified Value Platform combines the industry’s most robust cost, quality, and outcomes performance analytics with precise financial insights into a single source of truth that enables payers and providers to drive better care and outcomes.
Read More: Allbound Has Been Named A Leader In The G2 Summer 2021 Grid® Report For Partner Relationship…
“We are delighted by the synergy between Apervita’s Value Optimization Solution and Clarify’s analytics platform, which will unleash a ground-breaking end-to-end solution”
“Our health plan and value-based customers’ needs are increasingly complex, driven by intricate analytics requirements across multiple provider contract types. A trusted platform that can objectively and transparently analyze data from plans and providers is a foundational enabler to the success of new payment models. We are excited to welcome an experienced team that will further accelerate Clarify’s delivery of innovative payments and clinical improvement solutions,” said Jean Drouin, MD, CEO, Clarify Health.
The acquisition of Apervita’s Value Optimization business comes on the heels of Clarify Health’s $115M Series C funding led by Insight Partners. Since its creation, Clarify has generated more than 18 billion AI-powered predictions that have helped healthcare organizations improve the care of over 65 million members and patients. The Unified Value Platform will draw upon 300M+ payer-complete, longitudinal patient journeys, built from one of the largest and cleanest data sets in the industry, linking government and commercial claims, electronic health records, prescription, and social and behavioral data at the patient level.
“This deal reaffirms Clarify’s deliberate strategy to combine healthcare expertise with the latest technologies from other industries to create novel solutions that empower healthcare organizations to deliver better care and therapies. Our engineering and development teams are excited to offer healthcare organizations the full flexibility, precision and automation of payments capabilities more traditionally associated with financial services, the industry from where many of Clarify’s core engineers originate,” added Todd Gottula, President, Clarify Health.
“We are delighted by the synergy between Apervita’s Value Optimization Solution and Clarify’s analytics platform, which will unleash a ground-breaking end-to-end solution,” said Kevin Hutchinson, CEO of Apervita. “Health plans and providers need to be able to track and manage provider performance transparently with equal access to the performance data in real-time or near real-time. The combination of Apervita’s value-based payments reconciliation capabilities with Clarify’s cost, quality, and outcomes performance insights immediately delivers the leading value-based payments and clinical performance assessment solution in the industry.”
Read More: SAP Positioned As A Leader In 2021 Gartner Magic Quadrant For Multiexperience Development Platforms…
Apervita will continue to focus on providing solutions to support the industry’s transformation to digital quality measures and the rollout of clinical intelligence solutions that inform decision making at the point of care and can improve performance against those quality measures. This focus will enable Apervita to help health organizations address two trends in the marketplace. First, regulatory bodies like the Centers for Medicare and Medicaid Services (CMS) and National Committee for Quality Assurance (NCQA) have accelerated the transition to all digital quality measurements by 2025. Second, the pandemic made evident the need to support providers with real-time clinical insights and best-practice guidelines. Currently, more than 3,500 hospitals use Apervita’s Quality Measurement Solutions through a strategic partnership with The Joint Commission. Apervita will continue to transform quality measurement and care delivery by providing new capabilities to payers and providers, and enabling the Learning Health System, a framework that drives better outcomes and cost efficiencies across the health ecosystem.